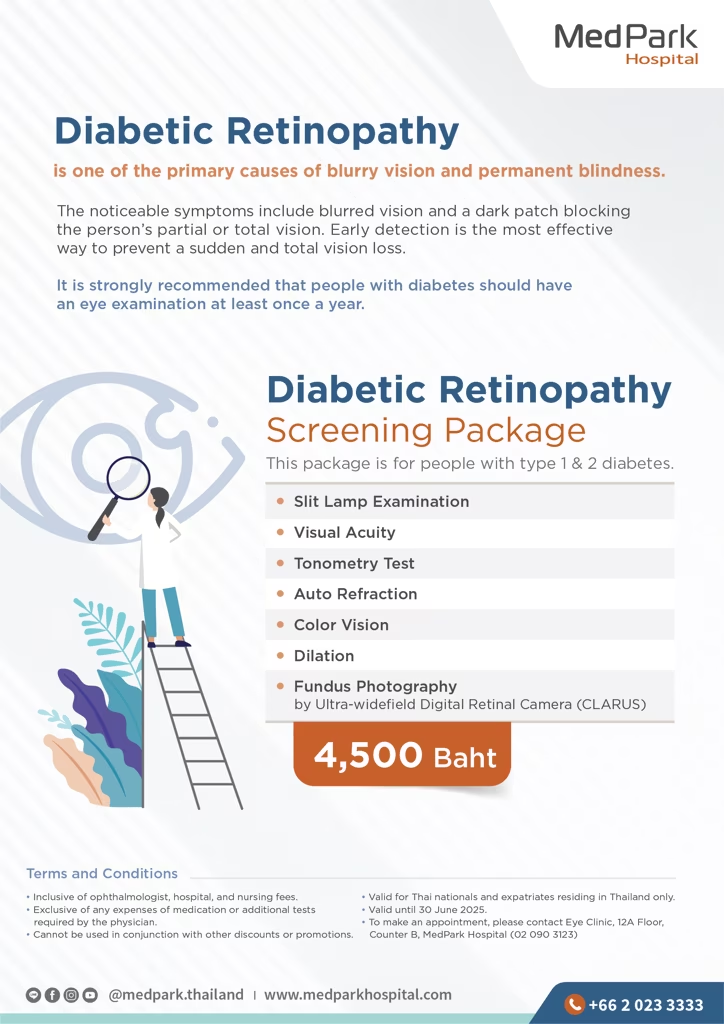
Diabetic Retinopathy Screening Package
Diabetic Retinopathy is one of the primary causes of blurry vision and permanent blindness. The noticeable symptoms include blurred vision and a dark patch blocking the person's partial or total vision. Early detection is the most effective way to prevent sudden and total vision loss.
It is strongly recommended that people with diabetes should have an eye examination at least once a year.
This package is for people with type 1 & 2 diabetes.
- Slit Lamp Examination
- Visual Acuity
- Tonometry Test
- Auto Refraction
- Color Vision
- Dilation
- Fundus Photographyby Ultra-widefield Digital Retinal Camera (CLARUS)
Terms and Conditions
- Inclusive of an ophthalmologist, hospital charges, and nursing fees.
- Exclusive of any expenses of medication or additional tests required by the physician.
- This package cannot be used in conjunction with any other discounts or promotional offers or a third-party payer such as an insurance company or contract company.
- The prices are valid for Thai nationals and expatriates residing in Thailand only.
- Please make an appointment in advance.
- No refunds under any circumstances.
Eye Care Center
12A Floor, Counter B
Tel. 02-090-3123